Severe Asthma
Understand what severe asthma is and how it is diagnosed and treated.People with asthma always have some underlying inflammation in the airway that can usually be treated with a combination of quick-relief and long-term controller medicines. But some people may not respond well to inhaled corticosteroids or other long-term controller medicines, a sign that they may be suffering from severe asthma. This inflammation may be more difficult to treat and requires testing to find the root cause of the inflammation. By working with your physician, you should be able to develop a custom approach for treating your asthma.
Diagnosing Severe Asthma
People with asthma may have ongoing symptoms and flare-ups, but that doesn’t necessarily mean they have severe asthma. Of the more than 25 million people in the U.S. living with asthma, only about 5-10% suffer from severe asthma. That is why it is important to talk to your doctor to determine if your symptoms signal severe asthma or are just uncontrolled asthma.
Uncontrolled asthma is often defined by the frequency of symptoms. For example:
- Daytime asthma symptoms (e.g., shortness of breath, chest tightness, cough) more than twice a week
- Waking up at night with asthma symptoms more than twice a month
- Using quick-relief medicine for symptoms more than twice a week
- Limiting activity because of asthma
Having three or more of these issues puts people with asthma into the uncontrolled category. These individuals could better control their symptoms by working with their asthma healthcare provider and discussing any issues with medication, reviewing inhalation techniques for medicines, and determining asthma triggers. Together, they should develop a plan to limit or avoid triggers and adjust their asthma treatment plan, such as adding a long-term controller medicine.
Difficult to Treat Asthma
People whose asthma remains uncontrolled despite using high dose controller medicines are described as having difficult to treat asthma. Factors that may make an asthma patient more difficult to treat are having another chronic health condition, incorrect inhaler technique, and/or inconsistent use of prescription medicine.
Severe Asthma
Patients with severe asthma use the highest dose of inhaled corticosteroids plus a second controller and/or oral corticosteroids. However, despite using high dose medicines, reducing risks, and following their treatment plan, many times their asthma remains uncontrolled. Severe asthma is categorized into three types: allergic asthma, eosinophilic asthma and non-eosinophilic asthma.
Testing for Severe Asthma
Before you can be tested for severe asthma, you will need a referral from your primary healthcare asthma provider to either an asthma specialist (pulmonologist) or allergy specialist (allergist). The specialist will review your medical history, your current asthma treatment plan and do a physical exam to assess your symptoms. If the specialist thinks you may have severe asthma, they will discuss additional testing with you to determine your specific type. This often starts with testing to identify a biomarker.
Biomarkers help determine what is causing the inflammation in your airways. Taking a blood sample, analyzing a mucus sample (sputum) or taking a breathing test that measure substances in your breath droplets are all common tests doctors use. These tests are performed in a doctor’s office or an outpatient clinic setting. Your specialist will recommend one or more of these tests based on your medical history and current symptoms.
Once the biomarkers are identified, your doctor can determine the type of severe asthma and the different treatment options that are available to treat that specific type.
Your physician should discuss the tests and treatment options with you so together, you can make a decision based on what you both agree will work best for you.
Below is a chart that describes the biomarkers for severe asthma, the testing method, the type (or phenotype) and the available possible treatment options for targeted therapy.
Biomarker | Testing method | Phenotype | Available treatments |
|---|---|---|---|
IgE* | Blood | Allergic (early onset) | Omalizumab |
Eosinophil | Blood | Eosinophilic (late onset) | Mepolizumab |
Neutrophil | Sputum | Neutrophilic | Antibiotics Lifestyle changes |
*IgE - immunoglobulin E
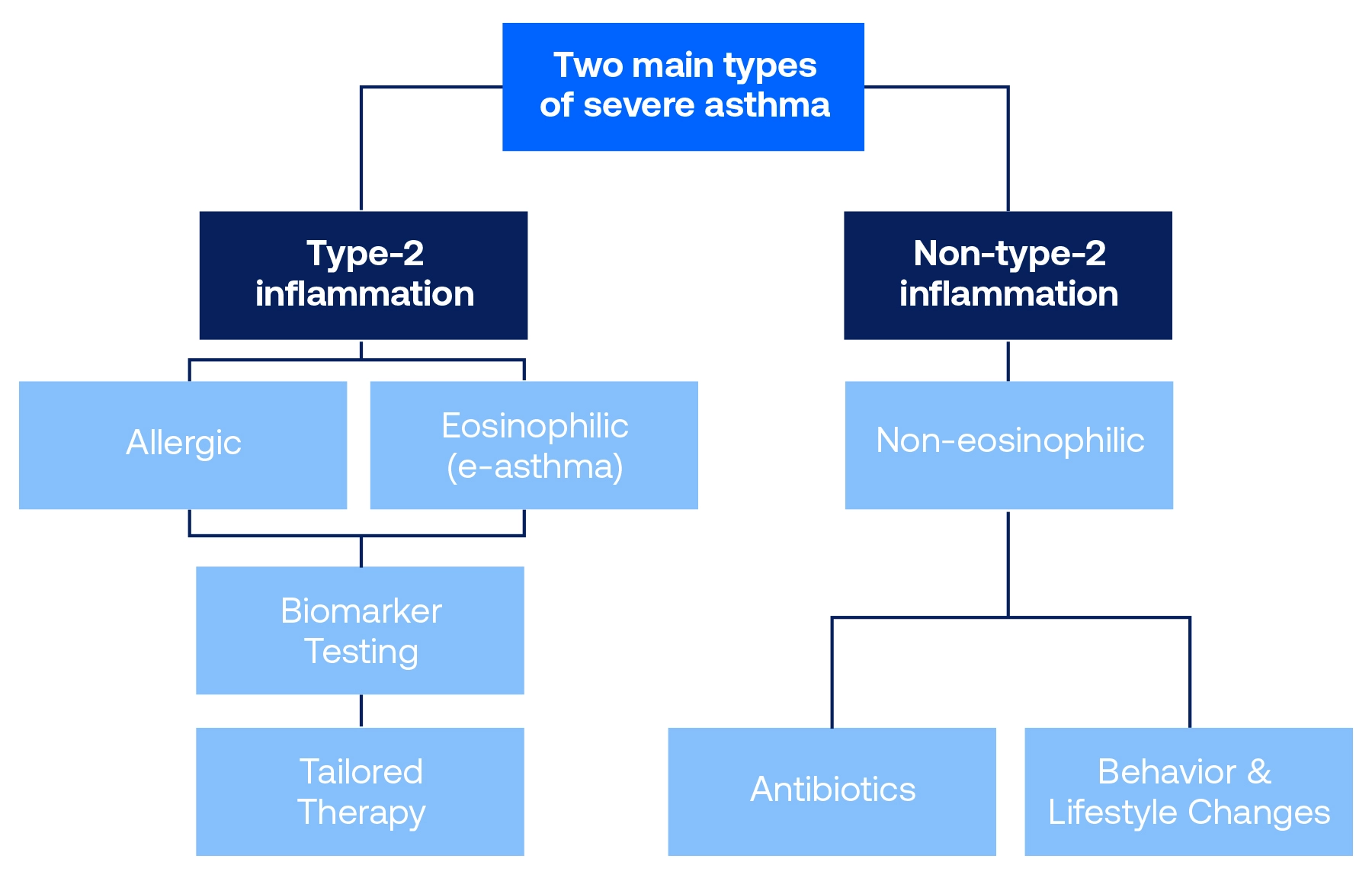
Types of Severe Asthma
There are two main categories of severe asthma—Type-2 inflammation and Non-Type-2 inflammation. These categories are based on a person’s response to treatment. Type-2 inflammation includes allergic asthma and eosinophilic asthma (or e-asthma) and Non-Type-2 inflammation includes non-eosinophilic asthma. For example, allergic asthma and e-asthma respond to treatment with inhaled corticosteroids and IgE (biomarker immunoglobulin E)-directed therapy or other biologics listed in the above table. Patients with Non-Type-2 inflammation, including non-eosinophilic asthma, generally do not respond well to inhaled corticosteroids. Allergic asthma and e-asthma have distinct biomarkers and treatment options available today. Treatments for non-eosinophilic asthma are currently being developed.
How to Treat Severe Asthma
Once your asthma specialist has determined the type of severe asthma you are suffering from, they can tailor treatment based on your specific type.
Basic treatment for severe persistent asthma consists of inhaled corticosteroids. Additional long-term controller medicines, such as long-acting beta 2 agonists (LABA), montelukast or theophylline, are added if asthma is still uncontrolled. Oral corticosteroids can be added on to treatment if patients are still experiencing symptoms and flare-ups.
A personalized treatment plan may include:
New treatments are available for patients with severe persistent asthma whose asthma is not controlled with inhaled corticosteroids and long-acting bronchodilators. Below are types of severe persistent asthma and their available treatments.
Type of severe asthma | Available treatment |
Atopic or allergic asthma | Anti-IgE (omalizumab) Blocks IL-4 and IL-13 (dupilumab) |
Eosinophilic asthma | Blocks IL-5 (mepolizumab, reslizumab and benralizumab) Blocks TSLP (tezepelumab) |
Hyperreactive asthma | Bronchial thermoplasty |
Treatments for allergic or eosinophilic asthma are given as an injection or IV every two to eight weeks depending upon the dose and medication required. Bronchial thermoplasty is a treatment given through an outpatient procedure called a bronchoscopy (a flexible tube with a light on the end of it). The bronchoscopy allows a pulmonologist to introduce a catheter that applies heat to the inside of your bronchial tubes. This heat causes the smooth muscle around your bronchial tubes to decrease by 60-70 percent and your airways become "less twitchy" to triggers.
Download the Severe Asthma Treatment Decision-Making Worksheet and use our Severe Asthma Treatment Planning Tool to help you start a discussion with your specialist.
Page last updated: January 27, 2026